Prostatitis is an inflammation of the prostate that is caused by various infections. It often develops acutely and is accompanied by an increase in temperature up to 37–38⁰ C, pain in the perineum, and problems with urination.
Untreated acute prostatitis becomes chronic and in this condition is more common. In this case, the symptoms are less pronounced (pain in the lower abdomen, when urinating, sexual disorders, general weakening of the body) or completely absent. However, the consequences can be very serious. The inflammatory process is directly related to potency problems and is expressed in a decrease in libido, obliteration of orgasm.
An unattended infection drastically increases the chances of developing complications. In particular, it concerns diseases such as:
- pyelonephritis;
- cystitis;
- prostate abscess;
- BPH;
- sterility.
Such consequences can be avoided if you consult a doctor in time. Take care of your health now, and in return you will get excellent health, psychological comfort and increased self-esteem, the quality of sexual intercourse.
Causes of prostatitis
This question is relevant not only because many men face this problem, but also because most of them cannot understand where they got this disease from.
Causes of prostatitis in men:
- sexually transmitted infections
- Inflammatory diseases of the urethra caused by conditionally pathogenic flora.
- Sexual dysrhythmia is an irregular and unbalanced sexual life.
- Physical inactivity is a sedentary lifestyle.
- Urolithiasis disease.
- The presence of foci of chronic infection in the body (chronic tonsillitis, pharyngitis, sinusitis, proctitis and paraproctitis, etc. ).
- Alcohol abuse and spicy food.
- Constipation.
- Hypothermia.
- Pathology of the lumbosacral spine and spinal cord - due to a violation of the innervation and trophism of the prostate.
Why does prostatitis occur when infected with an STI? The causative agents of genital infections, especially such as gonococcus, trichomonas, chlamydia, ureaplasma and mycoplasma, initially affect the urethra in men, causing venereal urethritis. But, like any living microorganism, these infections actively multiply in favorable conditions for them, which are the mucous membranes of the urethra and prostatic ducts.
Of course, if the patient turned to a urologist or venereologist in time, passed tests for STDs, revealed the presence of a sexual infection and cured it, then there will be no reason for the appearance of prostatitis. Everything will end with recovery at the stage of previous urethritis. But with an advanced form of the disease, with a formal approach to the treatment of sexually transmitted diseases, when trying to cure only by taking broad-spectrum antibiotics in tablets and not cured as a result, microbes get into the posterior urethra. and prostate, causing inflammation, ie prostatitis, and is most often both primary-chronic. In this case, it is very easy to avoid the development of prostatitis, absolutely everything depends on the patient himself.
All you need is:
- Seek immediate medical attention at the first sign of urethral discomfort.
- Pass the tests recommended by the urologist for STIs
- Undergo comprehensive treatment of identified sexually transmitted infections
- Do control tests after treatment to determine the presence of a venereal infection not only in the urethra, but also in the prostatic secretion
- And it is best to undergo medical prophylaxis in the clinic after casual sex, even before the appearance of STD symptoms and protect yourself and your loved ones from sexually transmitted diseases in general, and as a cause of prostatitis, in particular.
Symptoms of prostatitis
How to recognize or suspect prostatitis in an ordinary person, because its symptoms are very similar to many diseases of the genitourinary system and even other organs? How does prostatitis manifest? What are their first signs and how they behave with the progression of the disease. We will talk about this in this article.
What other diseases can be confused with prostatitis:
- Sexually transmitted infections (STDs) are the most common situation when a man goes to see a venereologist after a casual relationship, thinking that he has an STI. And indeed, the prostate was swollen.
- Urolithiasis can give similar symptoms, but at the same time, it can cause an inflammatory process in the prostate.
- Cystitis is rare in men, but the symptoms are very similar to those of prostatitis.
- Pyelonephritis: Inflammation of the renal pelvis has some symptoms in common with inflammation of the prostate gland.
- Diseases of the scrotum (epididymitis, orchitis, varicocele): heaviness and pain in the scrotum can be due to these diseases, including prostatitis.
- Diabetes mellitus: Patients note increased urination, as in prostate diseases, but there is no slow flow and the volume of urine is normal or even increased.
- Other diseases of the prostate: cancer and adenoma (benign hyperplasia) of the prostate.
- Urethritis.
- Diseases of the rectum - fissures, hemorrhoids, tumors.
- Diseases of the lumbosacral spine.
To make a correct diagnosis, a urologist needs not only to be very knowledgeable about the symptoms of prostatitis, but also to be able to correctly prescribe tests and other diagnostic studies, as well as to be able to properly evaluate their results.
So, consider the signs or symptoms of prostatitis:
Group 1 is a pain syndrome. That is, the appearance of pain in the perineum, in the groin, lower abdomen, scrotum, penis, rectum, sacrum, coccyx, inner thighs. It can be just pain, tightness, pressure sensations, or rather sharp, throbbing, severe pains. Sometimes a man simply complains of some discomfort in these areas, both during and outside of urination. Severe pain often intensifies when he sits for a long time in a chair or in a car.
In chronic slow prostatitis, the pain may subside after intercourse. If inflammation is strongly expressed in the prostate or large calcifications (stones) have formed in the gland, pain during ejaculation is possible.
Group 2 symptoms: urination disorders. There is an increase in urination, first at night, then throughout the day. The stream of urine becomes slow, the volume of each portion decreases, the transparency of urine decreases, blood may appear. With severe inflammation of the prostate or fibrosis of the gland around the urethra, there is a pronounced difficulty in emptying the bladder. A man has to strain, wait a while to urinate.
Group 3 - violation of sexual function. In the early stage of prostatitis, there is some increased sexual desire, hyperexcitability, and premature ejaculation. Also, due to a decrease in the production of sex hormones, a decrease in libido occurs, an erection falls. A man cannot have sexual intercourse or, having begun, cannot finish it. But, even when ejaculation occurs, the orgasm is dull or hardly felt at all. If an erection or ejaculation is accompanied by pain, then the man himself rejects new contacts, which negatively affects his sexual function in the future due to prolonged abstinence. And this also leads to the progression of congestive prostatitis. A vicious circle arises.
Group 4: These are general symptoms. There may be an increase in body temperature, tiredness, weakness, irritability, which are associated with both the presence of an inflammatory process and hormonal imbalance, as well as failures in sexual life. Some patients experience hyperhidrosis (high sweating) of the inguinal region, redness of the glans penis.
With a sufficiently pronounced inflammatory process in the prostate from the urethra, there may be mucous or purulent discharge.
The clinical picture of each patient with prostatitis is individual. Not all groups of symptoms are necessarily present and not all of them can be pronounced. With a chronic process in the prostate, a blurred clinic and minor symptoms are observed, but this does not make it less dangerous for a man's health.
Therefore, if you notice any manifestations of prostatitis from the above, make an urgent appointment with a urologist. Do not delay in contacting a doctor, because even if the discomfort has passed, this does not mean that the inflammatory process has stopped. It just entered a dormant stage and will gradually undermine his health and destroy the prostate gland.
The best option is a preventive examination every six months by a urologist with diagnostic palpation of the prostate, microscopy of its secretion, ultrasound and blood tests for PSA. Thus, you protect yourself from the negative consequences of not only advanced chronic prostatitis, but also adenoma and prostate cancer.
Treatment of prostatitis
Modern methods of treating prostatitis include the following varieties:
- pharmacological treatment (prescription of antiviral and antifungal drugs);
- maintenance therapy (prescription of immunostimulating drugs, food supplements);
- urological massage (prostate massage);
- LOD therapy (a method that uses low pressure to restore potency);
- a set of special physical exercises for relaxation;
- recommendations of the doctor regarding nutrition, lifestyle, sexual relations.
In the treatment I use the best methods of the main medical centers and own developments, which give excellent results.
Congestive (congestive) prostatitis
The treatment of congestive prostatitis presents certain difficulties, since the causes of this type of inflammation of the prostate are the lifestyle and sexual activity of this man. Consequently, only the patient himself, and not the doctor, can directly influence these processes. But even in such a difficult situation, patients can be helped. For the treatment of congestive or congestive prostatitis, a special complex therapy has been developed that allows you to eliminate the effects of blood stagnation in the prostatic venous plexus and prostate secretion in its ducts and acini.
Treatment of congestive prostatitis
After a preliminary diagnosis, which includes:
- Prostatic secretion analysis for microscopy, STIs, cultures
- PSA blood test
- General urine and blood tests.
- blood chemistry
- Ultrasound of the prostate, its venous plexus.
- ultrasound of the kidneys
A diagnosis of chronic congestive prostatitis is established, a complex of drug treatment and the necessary procedures are determined, including:
- Prostate massage through the rectum is necessary to remove leukocyte plugs, mucus, and congestive inflammatory secretion of the prostate from the ducts of the glands. It is the main treatment procedure that also improves blood flow in the prostate gland, which serves as a factor in the fight against blood stasis.
The massage is performed by a urologist. Session duration from 30 seconds to 2 minutes. Quantity from 10 per course. The cost is 600 rubles.
Even if the patient does not have the opportunity to complete the full course of treatment for congestive prostatitis, he must attend at least 10 massage sessions. Taking medications alone does not give the desired effect in treating congestion in the prostate.
- Vibromassage of the prostate is a very good and effective procedure for the treatment of congestive prostatitis. With the help of a special device that creates vibration, a thermal and magnetic field, the blood supply to the gland improves, the attachment of leukocyte plugs to the walls of the prostatic ducts is weakened, which facilitates their removal during the subsequent finger massage. It is usually done just before a massage session.
- Magnetic laser therapy improves blood flow and gland trophism, removes inflammation products and relieves swelling. Many patients feel its effect in the first days of treatment in the form of decreased pain and a feeling of tension in the prostate area.
This treatment of congestive prostatitis has been established for a long time and has been used successfully for many years, constantly being updated, including new methods and modern approaches. Chronic congestive prostatitis can and should be treated, achieving long-term remission and significantly improving the quality of life of a modern man.
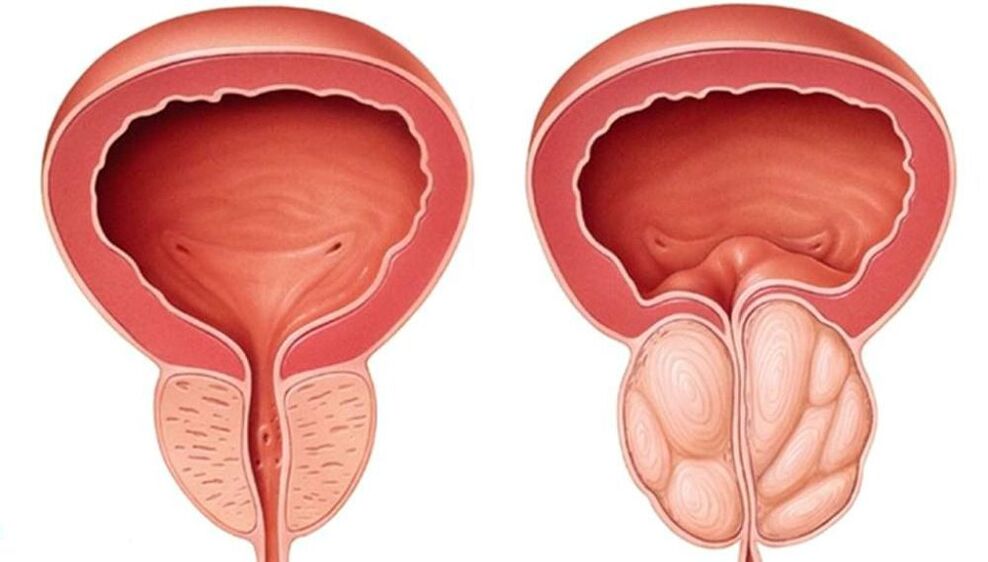
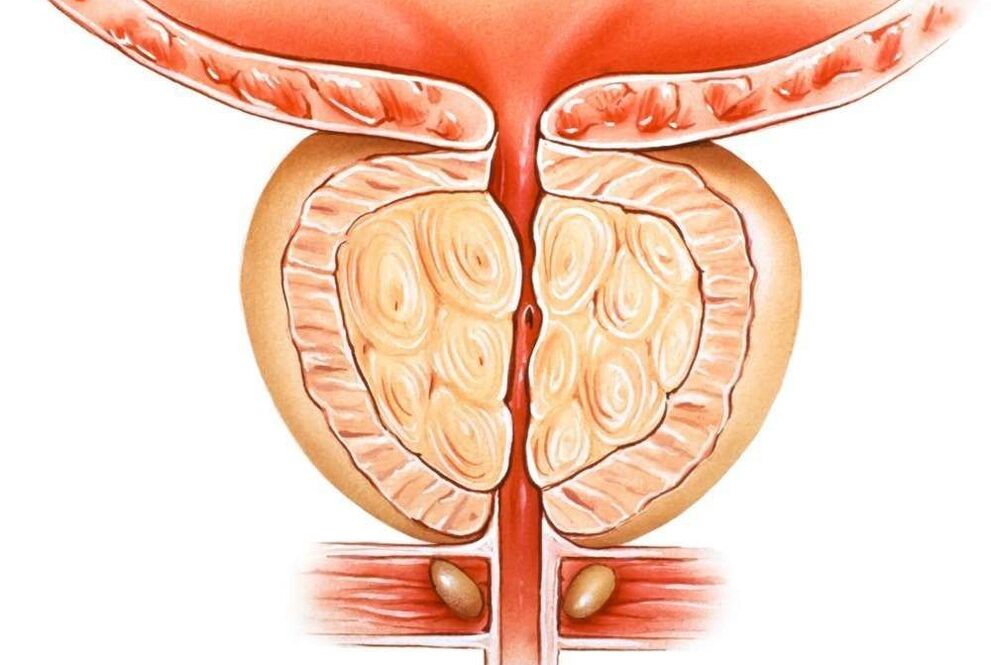
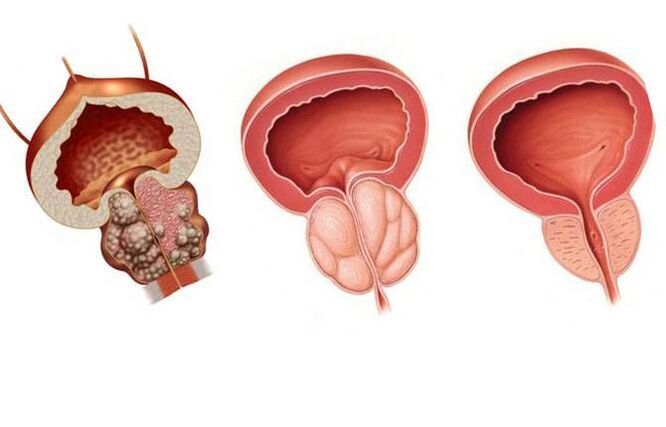
BPH
Prostate adenoma, or as it is now commonly called, benign prostatic hyperplasia (BPH) is a chronic disease that occurs mainly in older men, at least after the age of 50. After the age of 70, more than 50% of men already have complications from this disease. Although there are cases of its earlier development.
Prostate adenoma is accompanied by growth of its glandular and stromal (connective) tissue. As a result, nodules are formed in the thickness of the gland, which, when they reach a large size, begin to compress the surrounding tissues - the bladder, urethra, rectum, and sometimes the ureters, thereby disrupting the normal functioning of the gland. these organs.
Reasons for the development of prostate adenoma.
The development of prostate adenoma is associated with a hormonal imbalance in older men, that is, a kind of manifestation of "male menopause". Over the years, there is a decrease in the production of the main male hormone testosterone by the testicles and an increase in the content of the female hormone estradiol (especially in men with high body fat mass). A direct negative effect of female hormones on the prostate has been shown, as well as increased production of dihydrotestosterone in prostate cells, which causes active growth of its tissue and the development of benign prostatic hyperplasia, i. e. , adenomas.
Reasons leading to the development and progression of BPH may also include:
- hypodynamia - a sedentary lifestyle
- alcohol abuse and smoking
- fatty, high-cholesterol, spicy, spicy foods
- low sexual activity
Chronic prostatitis, in principle, is not the cause of prostate adenoma, but with a simultaneous course, it contributes to more pronounced symptoms and the rapid development of complications of prostatic hyperplasia.
Symptoms of prostate adenoma
Symptoms of prostate adenoma depend on the stage of the disease, its decompensation, the development of complications and the direction of tumor growth.
- First, there are signs of difficulty urinating, a slow stream of urine, constant urges up to 15-20 per day, nocturia - night urination.
- Then, as the bladder muscles weaken, pain in the lower abdomen worries, the feeling of incomplete emptying of the bladder, urine is excreted in portions, drop by drop, it is necessary to tighten the abdominal muscles. It ends with a complete loss of the detrusor, the bladder muscles that expel urine.
- When combined with chronic prostatitis, there is pain in the perineum, rectum, fever, discharge of mucus and pus from the urethra.
- Urine changes color, becomes cloudy, drops of blood may appear.
- Sexual function is impaired.
- With the growth of the prostate adenoma into the triangle of the bladder formed by the mouths of the ureters and the urethra, blockage of the ureters and a violation of the outflow of urine from the kidneys occur, which ends with a more rapid development of chronic kidney failure. failure and urolithiasis.
The main complications of prostate adenoma:
- Acute urinary retention: requires emergency bladder catheterization.
- As a result of stagnation of urine, urolithiasis and inflammation of the kidneys (pyelonephritis), bladder (cystitis) and urethra develop.
- The appearance of blood in the urine.
Chronic renal failure is a formidable complication that can lead to death.
Treatment of prostate adenoma
The clinic treats prostate adenoma without surgery, that is, drug therapy, which is more effective for stage 1 and sometimes 2 of benign prostatic hyperplasia.
Surgical treatment of prostate adenoma is performed with decompensation, growth of a large volume of prostate adenoma into the triangle of the bladder. It comes in different types:
- from an open transvesical adenomectomy - removal of the tumor through the bladder
- ending with minimally invasive methods, when through the urethra with the help of an electric scalpel, radio waves and laser techniques, the urethra is freed from the adenoma tissue or hyperplastic areas of the prostate are completely removed.
In order not to get to the fact that at the first visit to the urologist you are immediately offered an operation for prostate adenoma, it is necessary to undergo an annual examination of the prostate gland, an ultrasound scan and a blood test for PSA.
prostate massage
One of the most common and very effective diagnostic and treatment procedures in urology and venereology is prostatic (prostate) massage. This manipulation has long been used by urologists and is familiar to almost all patients with diseases of the prostate gland, seminal vesicles and STIs.
Why is prostate massage used?
Prostate massage can be used in two cases:
for diagnostic purposes for:
- Obtaining prostatic secretion for microscopic analysis
- Determination of the presence of sexually transmitted infections (chlamydia, ureaplasmas, mycoplasmas, gonorrhea, etc. ) in the prostate by PCR, PIF and others
- Take material for culture with determination of microflora and sensitivity to antibiotics
- Obtaining subjective data on pain, density, size of the gland - the so-called diagnostic palpation of the prostate.
for therapeutic purposes:
- to free the gland ducts of plugs of leukocytes and mucus
- to improve blood circulation in the prostate, which leads to better penetration of drugs into its tissue and the elimination of congestion
When is prostate massage prescribed?
Prostate massage is prescribed for a variety of men's health problems, including:
- chronic bacterial and abacterial prostatitis
- chronic vesiculitis - massaging the prostate and seminal vesicles
- chronic and slow urethritis
- prostatitis caused by genital infections
- erectile dysfunction and infertility associated with prostate diseases
- with preventive purpose in the treatment of STDs in their final stage
Prostate massage is not performed in the presence of acute purulent inflammation of the genital organs!
How is prostate massage performed?
There are several classic prostate massage positions.
The most common is the knee-elbow position, when the patient stands on the couch on his knees and arms bent at the elbow joints, bending at the waist.
In diseases of the spine, old age, large body weight, it is possible to stand on the left side with the legs bent at the knees, brought to the stomach.
When massaging the seminal vesicles, the patient stands with his feet on the couch with his back to the doctor and is in a semi-squatting position.
During prostate massage, the urologist's index finger is inserted into the patient's rectum and begins to alternately massage the right and left lobe of the prostate, ending with the interlobular groove (isthmus). During this manipulation, which lasts from 30 seconds to 2 minutes, the doctor receives information about the pain of the gland, its size, consistency, surface, severity of the groove, and can take the secret of the prostate for analysis.
During prostate massage, there may be some discomfort, urge to urinate, feeling of pressure in the lower abdomen, penis. With severe pain, the massage is stopped.
It is very important that this procedure is performed by qualified experienced urologists or venereologists so as not to harm the man and not injure the prostate.
Vibromassage of the prostate

Vibromassage of the prostate: the use of vibration, magnetic field and heating in the treatment of chronic prostatitis. This type of physiotherapy improves the blood flow and nutrition of the prostate tissue. Vibromassage helps remove leukocyte plugs from the gland ducts. With calculous prostatitis - one of the alternatives to finger massage. The duration of the session is from 10 to 20 minutes.
Prevention of prostatitis
Prevention of prostatitis consists of avoiding the predisposing factors that cause prostatitis, as well as:
- Try not to freeze for a long time, if you have a long stay in a cold room or on the street, take care of proper clothing.
- For constipation, use laxatives and do not torture yourself.
- If you have a sedentary job, take an "exercise break" every hour (or at least just get up and walk around).
- Try to have a regular sex life, as this is fully compatible with a person's normal lifestyle and allows you to avoid many problems, not just prostatitis.
- Try to eat regularly and well, maintain an active lifestyle, do not get sick, and finally just think about your health from time to time.
And also do not forget to visit a urologist regularly.























